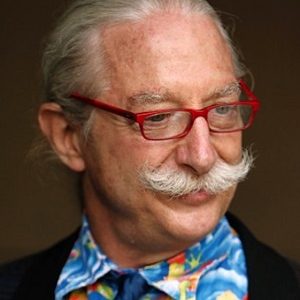
One of America’s Premier Healthcare Futurists
Jeff Goldsmith is President of Health Futures, Inc and National Advisor, Navigant Healthcare. For eleven years ending in 1990, Jeff Goldsmith was a lecturer in the Graduate School of Business at the University of Chicago, on health services management and policy. He has also lectured on these topics at the Wharton School of Finance, Johns Hopkins, Washington University and the University of California at Berkeley. Jeff Goldsmith’s interests include: biotechnology, health policy, international health systems, and the future of health services.
Healthcare Advisor
From 1982 to 1994, Jeff Goldsmith served as National Advisor for Healthcare for the firm Ernst and Young, and provided strategy consultation to a wide variety of healthcare systems, health plans, supply and technology firms. Prior to 1982, he was Director of Planning and Government Affairs at the University of Chicago Medical Center and Special Assistant to the Dean of the Pritzker School of Medicine. From 1973 to 1975, Jeff Goldsmith worked in the Office of the Governor, State of Illinois as a fiscal and policy analyst, and Special Assistant to the State Budget Director.
Education
Jeff Goldsmith earned his doctorate in Sociology from the University of Chicago in 1973, studying complex organizations, sociology of the professions, and politics of developing nations. He graduated from Reed College in 1970, majoring in psychology and classics, earning a Woodrow Wilson Fellowship for graduate study in 1971.
Awards
Jeff Goldsmith was the recipient of the Corning Award for excellence in health planning from the American Hospital Association’s Society for Healthcare Planning in 1990, and has received the Dean Conley Award for best healthcare article three times (1985, 1990 and 1995) from the American College of Healthcare Executives.
Publications
He has written six articles for the Harvard Business Review, and has been a source for articles on medical technology and health services for the Wall Street Journal, the New York Times, Business Week, Time and other publications. Jeff Goldsmith is a member of the editorial board of Health Affairs.
Jeff Goldsmith is the father of two sons and a daughter. He is an avid snow skier and collects Native American art and artifacts. He is married to Karen Walker, a florist in Charlottesville, who owns Hedge Fine Blooms, specializing in fresh flowers and cutting edge floral design for businesses, weddings and events. Jeff Goldsmith is a native of Portland, Oregon and lives in Charlottesville, Virginia.
What Makes a Health System?
Health care organizations have grown steadily larger and more complex over the past thirty years. Most of them call themselves “health systems”. But are they really systems and have patients and those who pay for care benefited from this growth and complexity? Why has “health system” operating performance deteriorated sharply since the historic Affordable Care Act coverage expansion? How can health systems make changes in their operations and management that patients notice? What does it mean to be a health system? Opiate Crisis: Tip of a Population Health Iceberg: In 2016, more than sixty thousand Americans died of drug overdoses, 42 thousand from opioids. Drug death are the SuperStorm Sandy of public health threats, likely to claim more victims than the AIDS Epidemic. Yet it is the most visible manifestation of a more troubling trend-declining American life expectancy. In both 2015 and 2016, American life expectancy declined, the first two-year decline since the early 1960’s. During the same two years, the US spent nearly $7 trillion on healthcare. What are the underlying drivers of this deeply troubling trend., and what can policymakers and the care system do about it?
What Will the Trump Presidency Bring to Healthcare?
Donald Trump won an unexpected Presidency in part by promising to repeal ObamaCare, the landmark 2010 Obama administration health reform law. This law provided coverage for 20 million formerly uninsured people and hundreds of billions in new funding for hospitals and care systems. How will unwinding and replacing this law affect those who render care? What role did poor health play in Trump’s election? How will a divided Republican Party decide where to cut and how to restructure Medicare and Medicaid, the twin mainstays of public funding for health services? Where will Trump succeed and where will he fail? What strategies best position hospitals and physicians to cope with a new wave of policy uncertainty?
2037: A Healthcare Odyssey
In 1986, in Hospitals’, Jeff Goldsmith looked ahead fifty years to the US healthcare system in 2036. In 2016, Jeff revisited these forecasts, noting both accurate and inaccurate predictions, and looked ahead yet again to the health system in twenty years time. In 2037: A Healthcare Odyssey, Jeff examines the digital health revolution he foresaw in his 1986 piece, and how it is likely to affect care. He also looks at the concluding chapter of the baby boomer’s saga, as well as promising new progress in the neurosciences and produces a fresh forecast for the US health system in twenty years.
The Tragedy of Health Reform
Despite compelling unmet needs, the bold health reforms enacted in 2010 in the Affordable Care Act appear to be faltering. A lethal combination of political controversy, flawed design and incompetent implementation have put health reform in peril. What went wrong? How will the unfolding of expanded health coverage, increased regulation and new models of care and coverage affect the health system and society? Will employers abandon health coverage and push their employees into the Exchanges? Will the Exchanges revitalize or destroy private health insurance? How will health reform affect caregivers and patients? Will the Medicaid program sustain a 20% increase in enrollments? Can or should health reform be saved? A veteran health policy analyst looks at ObamaCare and looks ahead. Slouching toward Value: The Future of Health Care Payment: One major theme of health reform has been to change how healthcare is paid for to reward higher value care. In a $2.8 billion industry, the uncertainty about future payment models has created confusion about strategic direction in hospitals and systems, physician communities and health insurers, as well as anxiety among patients and their families. Ironically, a Democratic health reform has produced Republican outcomes- high degrees of consumer economic exposure, narrowing networks, and a welter of confusing new choices. Meanwhile, new payment models- pay for performance, bundled payment, accountable care organizations, patient centered medical homes- have been given fresh impetus. How will all these experiments turn out? How SHOULD healthcare be paid for? This talk focuses on the winners and losers in the search for more accountable and affordable care, and the models and strategies that are likely to prevail.
Can Hospitals Survive? Hospital Strategy in a Maturing Market
After decades of seemingly continuous expansion, hospital inpatient utilization in the United States has fallen for five years in a row. Despite forecasts a decade ago of significant bed shortages, many hospitals and systems find themselves with excess capacity. At the same time, the uncertainties surrounding ObamaCare and the pressures created by the recession have stressed hospitals, resulting in declining earnings and increased pressure from physicians and patients. Merger and acquisition activity spiked after 2010’s health reforms, and continues unabated. How will the private insurance reforms contained in ObamaCare affect hospitals’ financial futures? Can hospital systems that have sought to become “unavoidable” through mergers survive the transition to narrow network insurance products and rising transparency and consumer choice? Can hospitals survive this transition? How can hospitals become the “hospitals of choice” in their communities and regions.
Changing of the Guard: How the Impending Generational Transition among Physicians will Change Medicine and Health Services
The present US health system is 'powered by baby boom physicians'. As these physicians gear down or retire outright, they are being replaced by younger physicians with different values, practice goals and communications styles. How will this generational transition affect medical practice, as well as hospital/physician relations? How will policymakers cope with the impending scarcity of practicing physicians as the baby boom itself enrolls in Medicare?
All Jeff Goldsmith Books

The Sorcerer’s Apprentice: How Medical Imaging Is Changing Health Care
Purchase Book
The Long Baby Boom: An Optimistic Vision for a Graying Generation
Purchase Book